New from FASEB BioAdvances: Tool Tracks Early Osteoarthritis Signals in Joints
Tuesday, October 8, 2024A fluorescent dye could help scientists listen in on biochemical conversations between cartilage and bone during the earliest stages of osteoarthritis (OA)—even before the disease causes pain. The unexpected finding could someday lead to novel treatments for patients, according to research conducted on mice that was published today in FASEB BioAdvances.
OA is a painful condition in which the cartilage layer in a joint wears away, causing bone to rub against bone. This articular cartilage also becomes calcified, turning into bone. The progressive condition is common among people 60 years of age or older, as well as those with certain metabolic diseases or who place repetitive stress on a particular joint. Although there is no cure, early interventions could help prevent further damage. However, it is difficult to detect OA in early stages before a patient feels pain.
Bin Wang and colleagues at the Sidney Kimmel Medical College of Thomas Jefferson University wanted to know whether articular cartilage becomes calcified early in OA, so they studied a mouse model in which the right knee exhibits symptoms similar to the human disease.
A fluorescent red dye called alizarin complexone binds calcium-containing crystals, and the researchers injected this dye into both knees. Surprisingly, there was no fluorescence staining on the surface of the articular cartilage layer—where the team expected to find new calcification—in early OA stages.
The tidemark area, a barrier between the articular cartilage and a layer of calcified cartilage that resides on the bone was stained in both knees. “But we found more of the alizarin dye in the calcified cartilage and subchondral bone in osteoarthritic mice compared to control,” says Wang. Increased diffusion of the dye suggests that the early-OA knee joint is more permeable than the control.
With an injection, dye first goes directly into the synovial fluid that cushions the joints. In additional experiments, the researchers found that the dye could then move throughout the joint via three expected pathways. However, they also observed a fourth, brand-new pathway into the blood vessels in the outer covering of the bone, called the periosteum, via the tidemark. The fluorescence signal was greater in the periosteum, as well as in the subchondral bone of early-OA mouse joints than in controls.
Taken together, the findings mean that “alizarin complexone is a new tool that can detect diffusion, or biochemical communication, from the articular cartilage to the calcified cartilage and subchondral bone,” says Wang. Compared to controls, diffusion is boosted in early stages of OA. With this tool in hand, researchers can now use it to better understand the progression of OA as a step toward developing new treatments. “This is just the beginning,” says Wang.
Funding: National Institutes of Health, Rheumatology Research Foundation
Read the full article, “New role of calcium-binding fluorescent dye alizarin complexone in detecting permeability from articular cartilage to subchondral bone,” published online in FASEB BioAdvances.
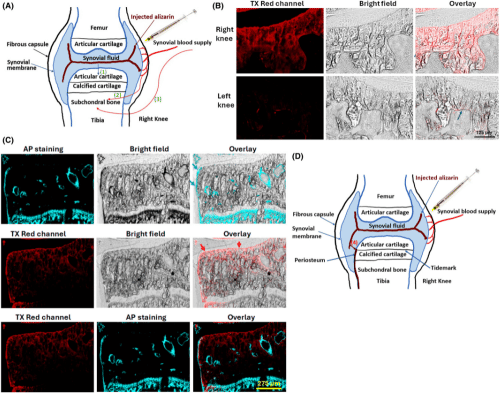
Figure 2
Alizarin complexone via the intra-articular injection can enter different directions in the joint.